Could Ignoring Exercise for Depression Be Psychiatric Malpractice?
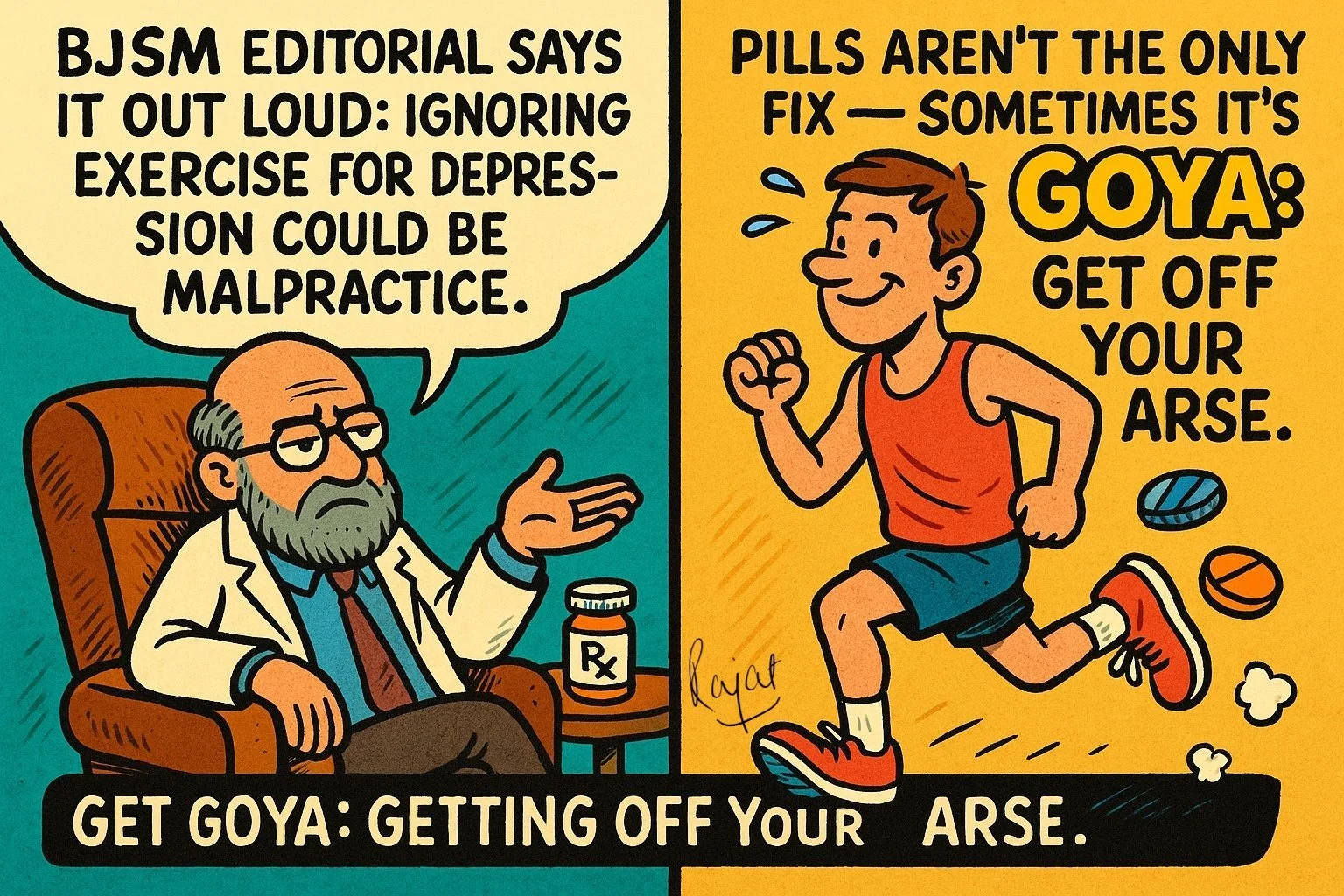
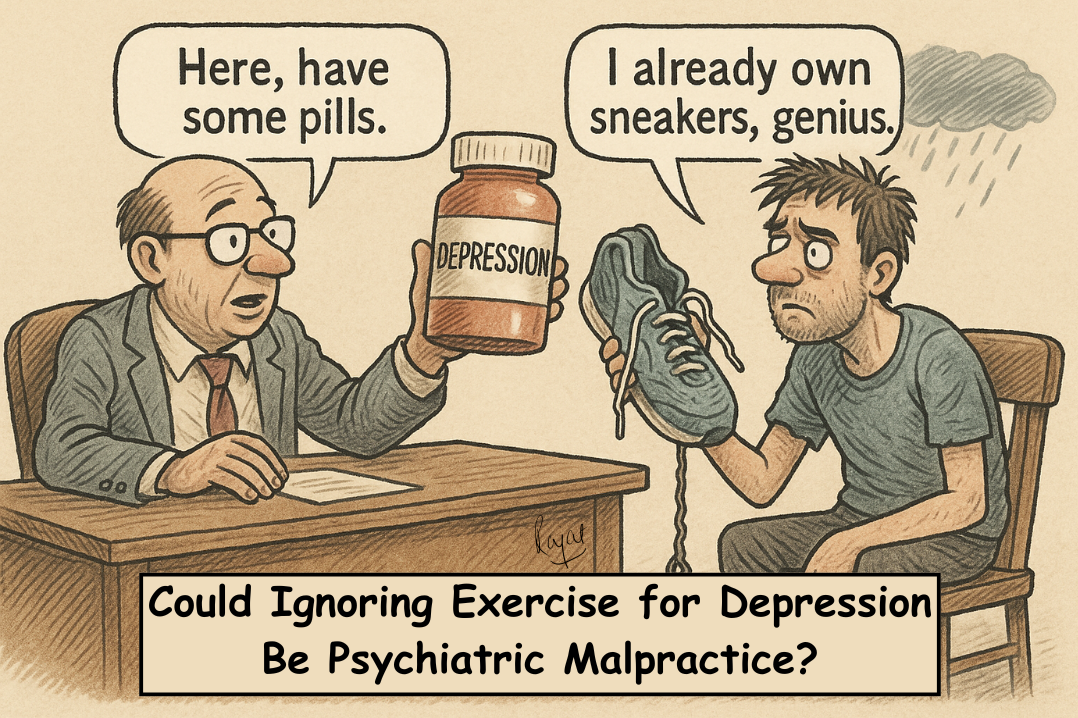
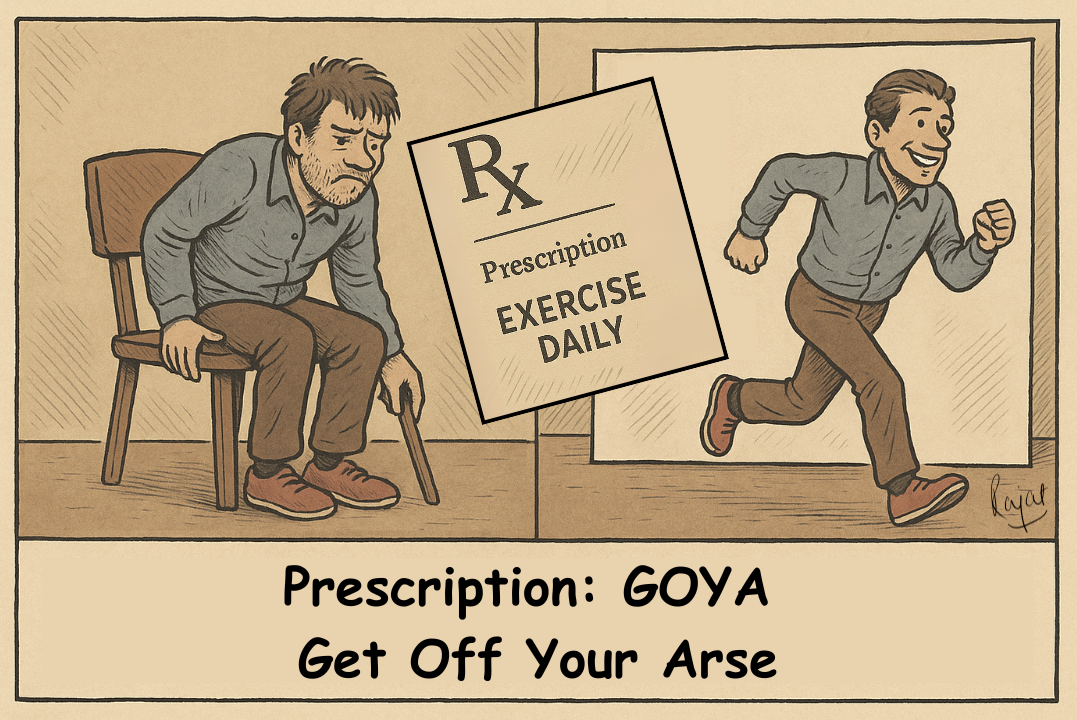
An editorial in British Journal of Sports Medicine (BJSM) recently asked a deliciously uncomfortable question: could not prescribing exercise for depression be psychiatric malpractice? Think about that for a second. For decades, psychiatrists have happily handed out pills or offered a couch and a sympathetic ear, but almost never the most obvious prescription of all: GOYA, Get Off Your Arse.
Which is odd, because exercise has been shown to lift mood just as well as medication or therapy, while also fixing the body along the way. Lower blood pressure, stronger heart, fewer suicidal thoughts. And the side effects? A fitter, more toned, and yes, even sexier, you. The best company you’ll ever have, both physically and mentally. And let’s be honest: if you can’t stand your own company, why should anyone else?
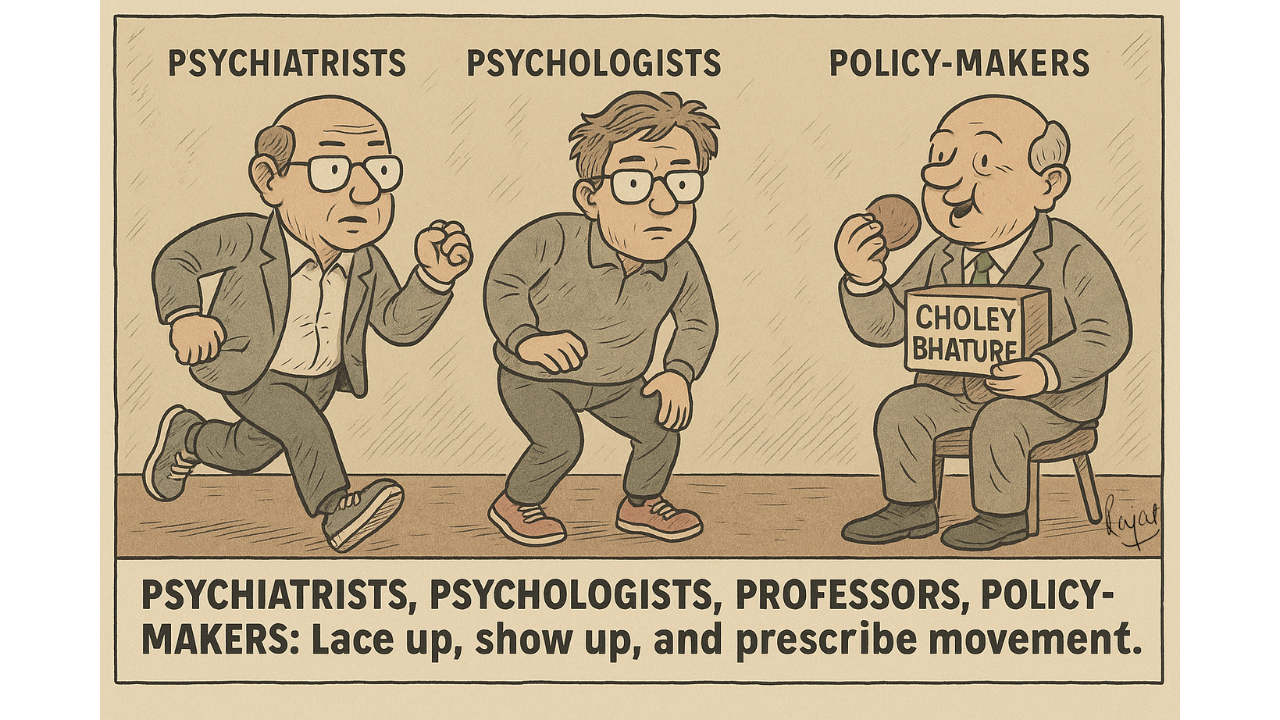
So why do psychiatrists, and even psychologists, act like they’re allergic to running, strength training, or any sport that might make their patients sweat?
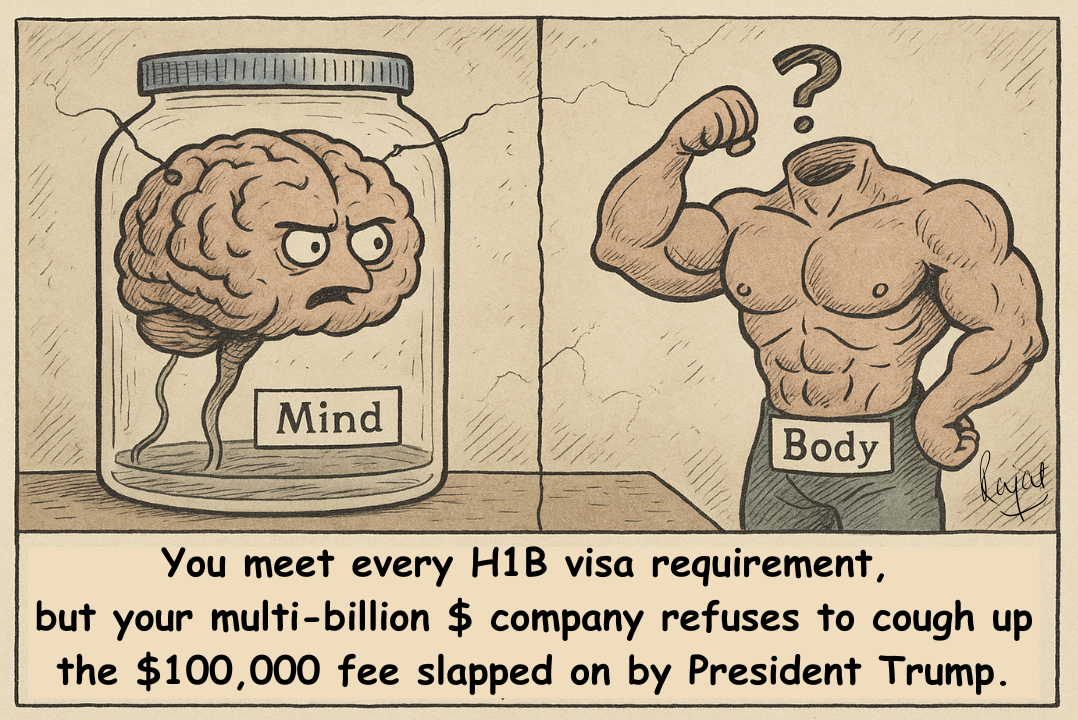
Mind and Body: The Great Divorce
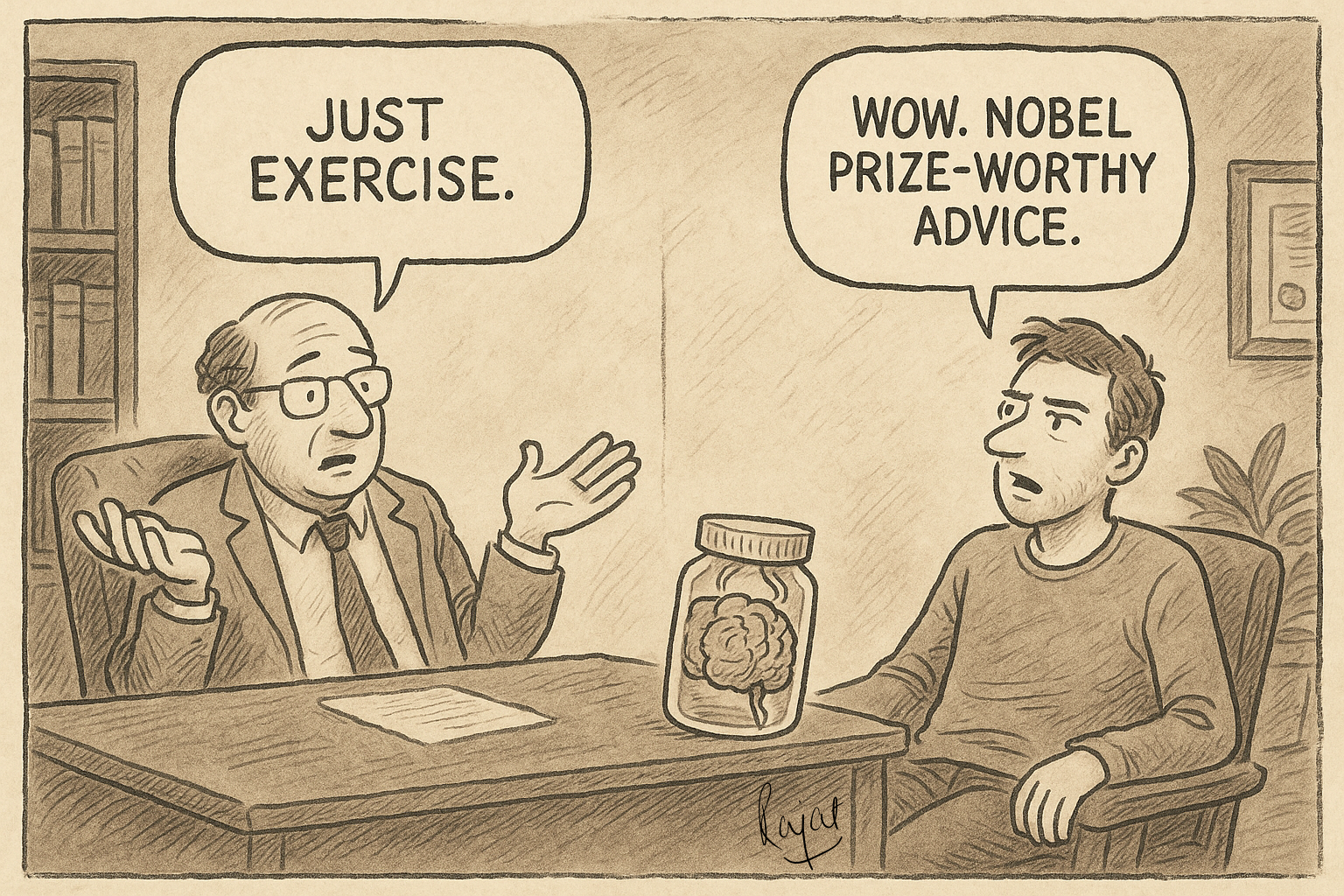
Psychiatry and psychology have long behaved as if the brain floats in a jar, disconnected from the body that drags it around. I once had a professor of psychology proudly tell me he cared only about the mind, the body was irrelevant. He wasn’t joking; he meant even his own body.
And doctors in other specialties aren’t any better. Cardiologists obsess about arteries, orthopedists about bones, as if the rest of the body were dead weight in the trunk, and the brain an optional upgrade you could buy later, like leather seats. The absurdity is breathtaking: depression wrecks both body and mind, yet we insist on treating them in isolation. It’s like meeting every H1B visa requirement, but your company refuses to cough up the $100,000 fee slapped on by President Trump.
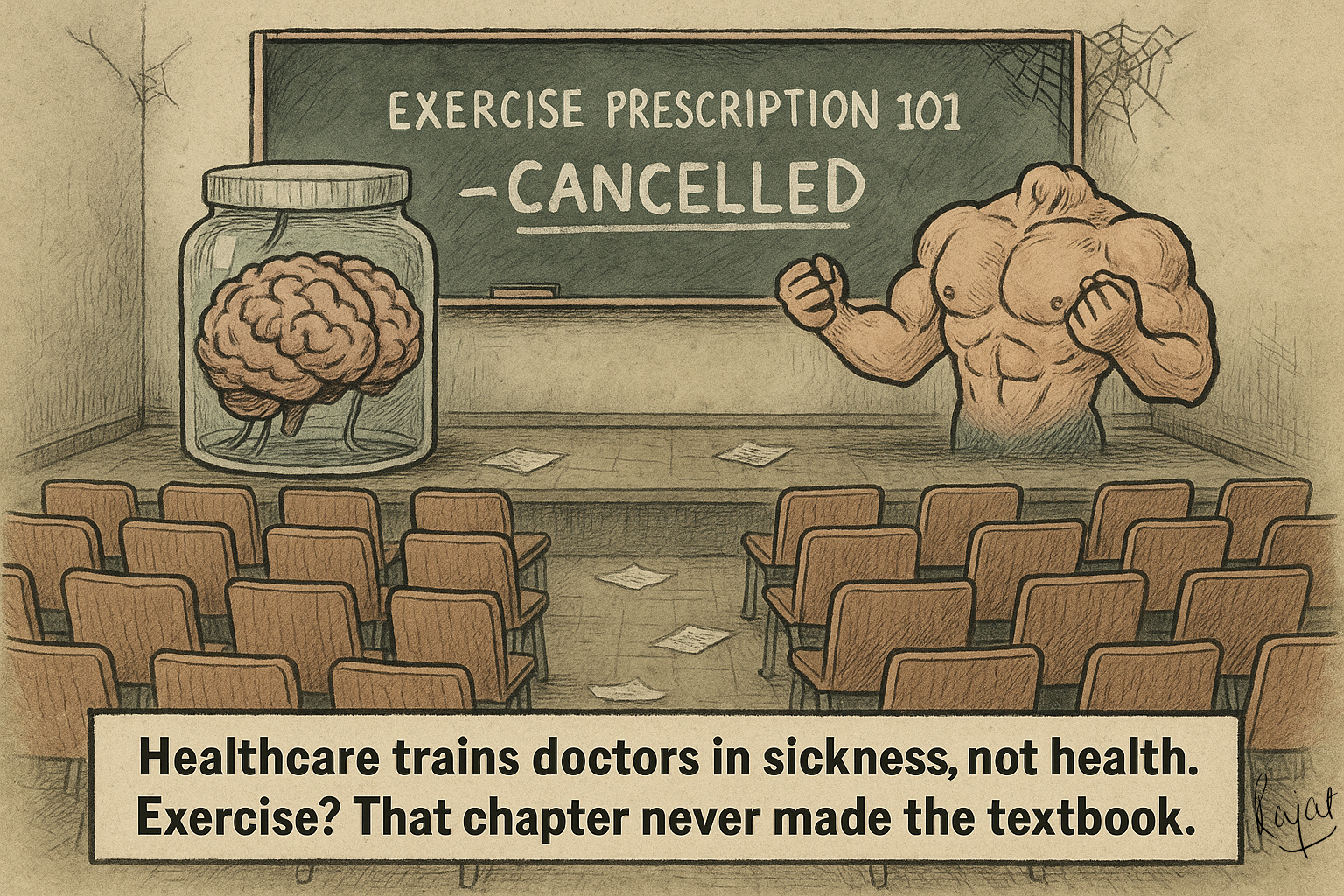
The 92% Problem
Here’s the punchline: 92% of mental health professionals admit they’ve never been trained to prescribe exercise. Honestly, I’d say it’s closer to 100%, the other 8% are probably lying. And this isn’t about lazy doctors, it’s about a lazy system. From the start, medical training is crammed with pathology, what goes wrong, and barely touches physiology, how the body works when it’s right. Which is crazy: if you don’t know normal, how can you recognise abnormal?
By the time doctors specialise, psychiatry, orthopaedics, whatever, their vision has narrowed to silos so tight they could choke. They’re taught to fix body parts or brain chemistry, not people. No wonder almost half of psychiatrists admit they never bring up exercise with patients. And the excuses? “That’s not our job.” Imagine an orthopedician recommending knee replacement surgery without even listening to your side of the story or looking at your knee. If the whole decision is based on an X-ray, why not just erase the “bad parts” on the film and call it fixed?
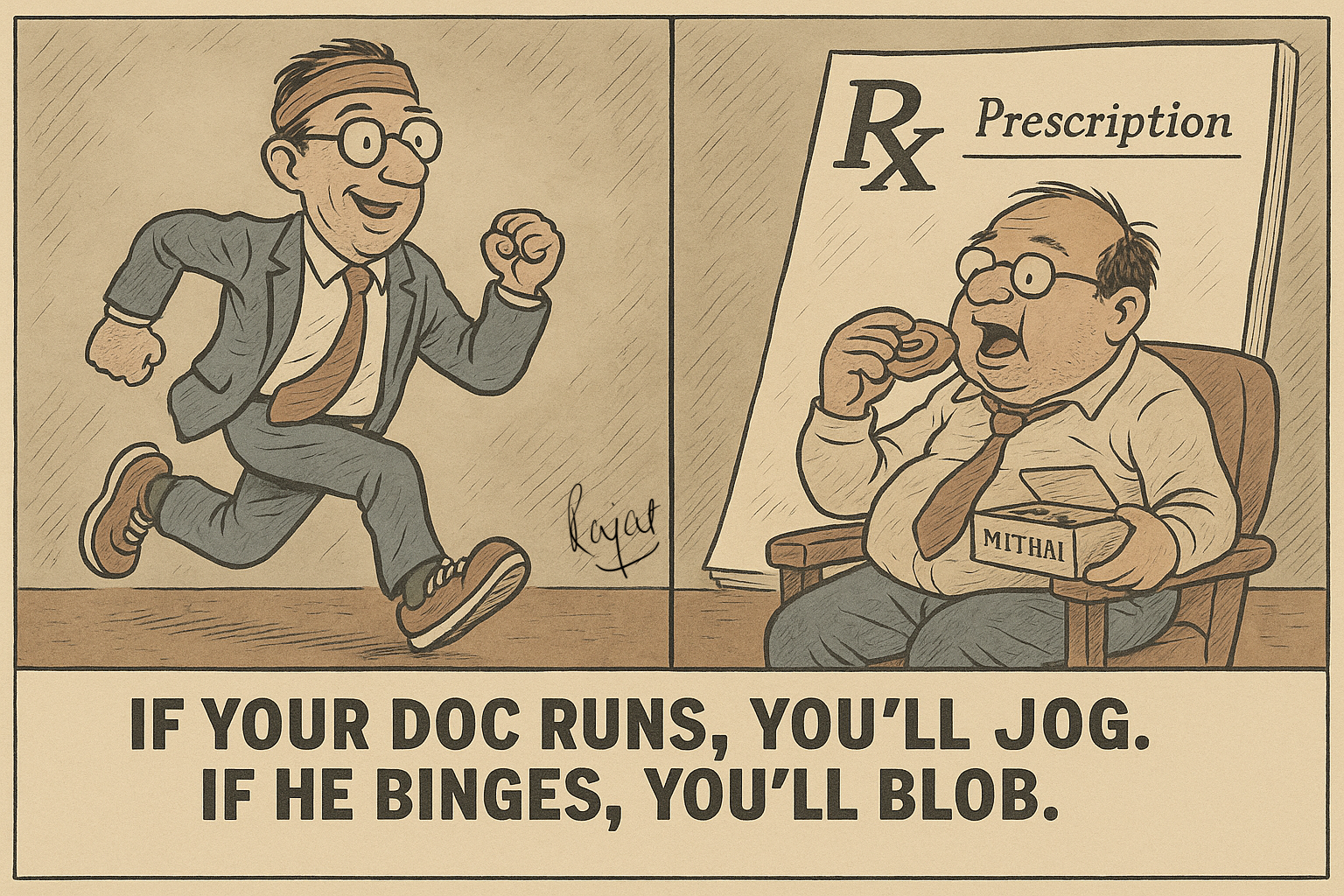
And here’s the irony: the psychiatrists who do recommend exercise are usually the ones who actually exercise themselves. Monkey-see, monkey-prescribe. If your shrink runs marathons or lifts weights, you’ll hear about jogging or strength training. But if their only sprint is to the mithai shop, and their version of weight training is lifting a jalebi to their mouth, don’t hold your breath for a workout plan.
Just Exercise! The Masterstroke?
Even when exercise does get mentioned, it’s usually tossed out like a magic spell: “You should try to be more active.” As if that spell alone will cure depression, reshape habits, and tone your thighs by sunrise. That’s about as useful as telling someone with depression to “just cheer up.” Or like the good old days when parents thought a slap could fix everything.
What’s missing is clarity. Exercise, to be useful, needs a bit of structure, not a 50-page training plan, just enough to make it doable. That’s where the FITT principle helps: Frequency, Intensity, Time, Type. “Brisk walk, 30 minutes, five days a week.” “Strength train, 30–45 minutes, three days a week.” Simple, clear, and practical. And if psychiatrists are active themselves, this comes naturally, they know what works and what doesn’t.
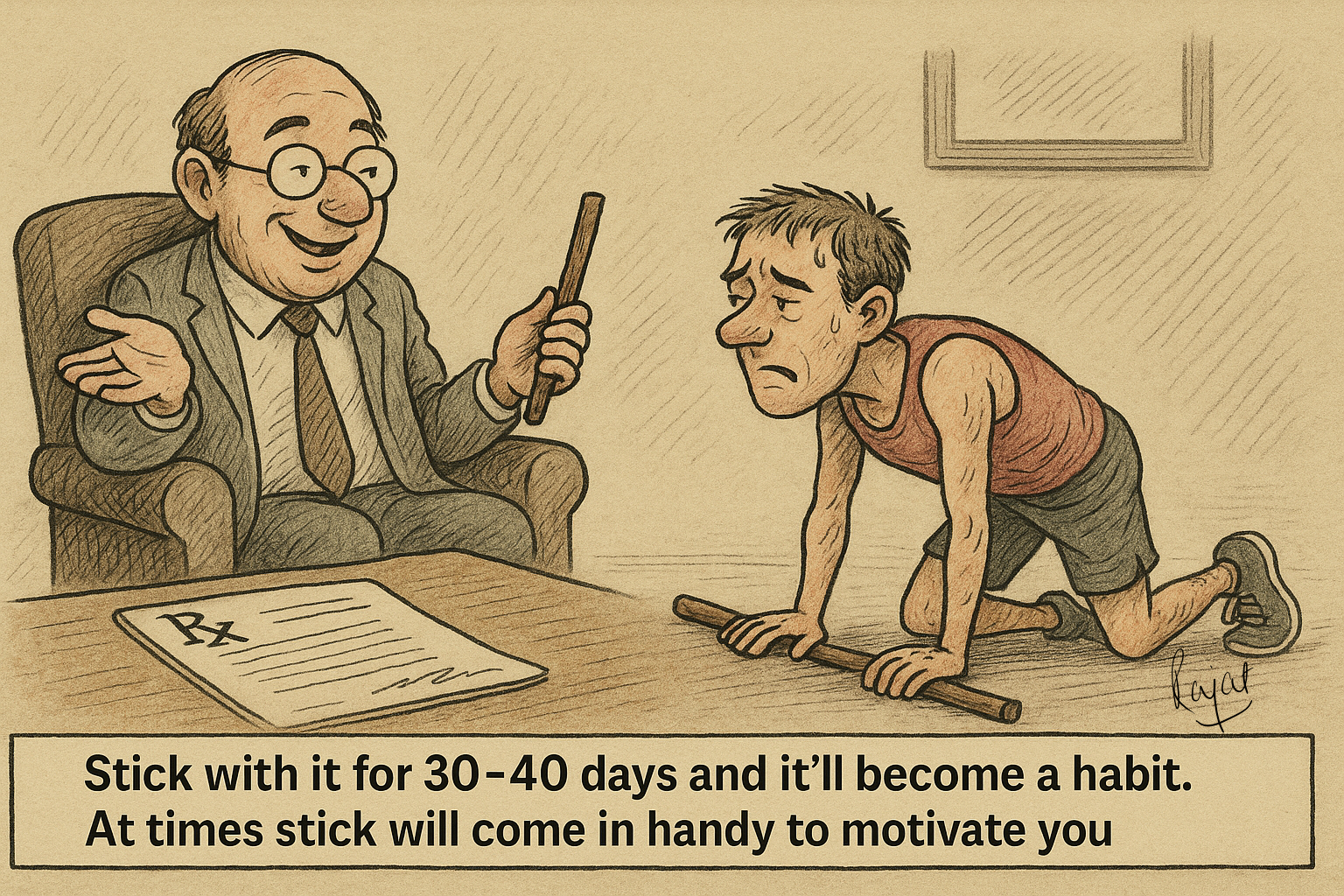
But here’s the catch: the best exercise plan is the one that actually gets done, not the one that looks fancy on paper. Doctors love parroting “3 sets of 10.” As if the universe suddenly transforms when you hit rep number 10. Newsflash: it doesn’t. You could stop at 9, push to 12, or do 2 sets instead of 3, the universe won’t implode. The only magic number is the one that keeps you coming back the next day. Hell, at the right intensity, even one set is enough. But that’s a rabbit hole for another blog. For now, “move more” is not a prescription, it’s a shrug.
And let’s not forget human nature: it takes 30-40 days to form a habit. The first few weeks aren’t about joy, they’re about showing up. Discipline beats passion, yours or theirs. Passion may light the spark, but discipline keeps the fire going. Which is why creating environments where people actually turn up is far more important than writing programs that look impressive but never get done.
Personally, for me, the biggest payoff of being active, whether it’s running, strength training, swimming, cycling, or playing any sport, is simple: joy. It’s fun. And fun is underrated. But to get to the fun, you first have to do the boring bit: just start.
Living Cadavers?
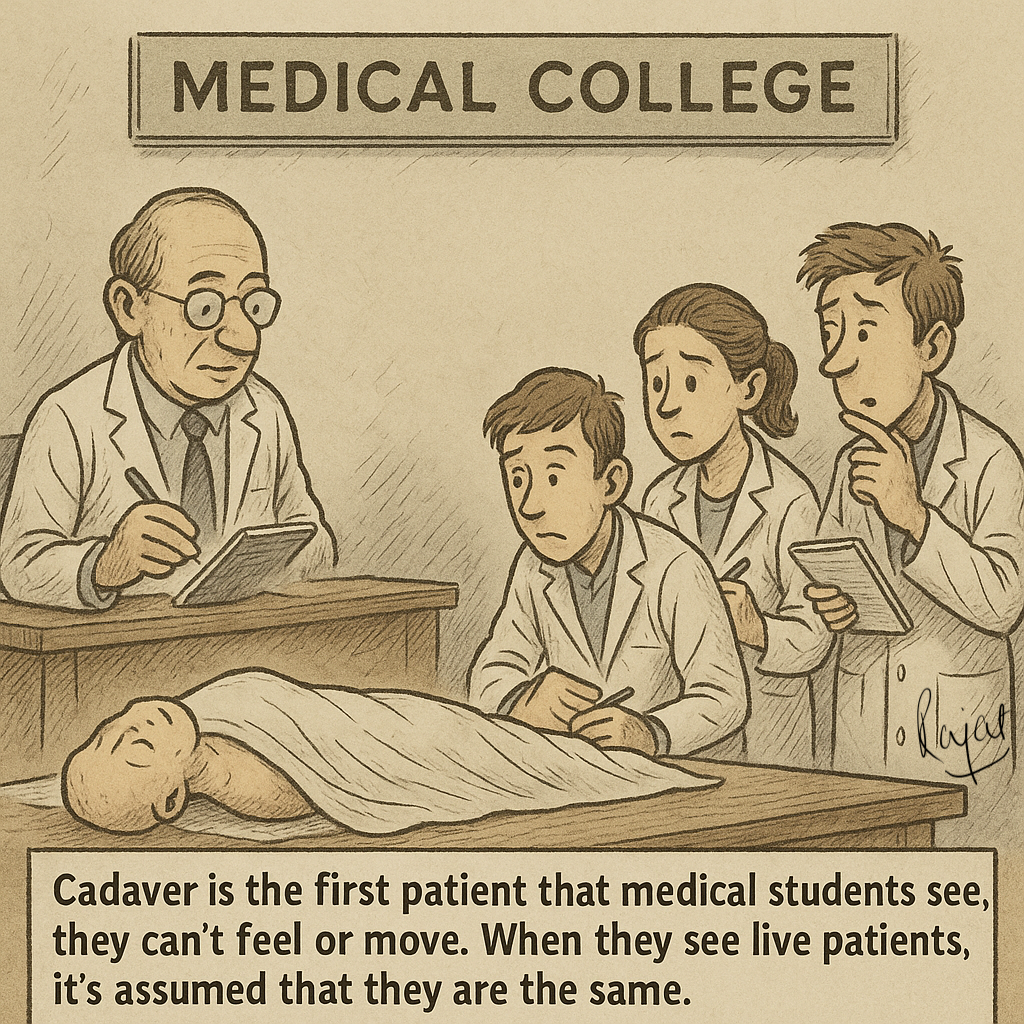
Maybe this blind spot starts in medical college. A medical student’s “first patients” are cadavers. They learn to poke, cut, and prod lifeless bodies, and yes, they learn a lot. But the subconscious message is brutal: patients are bodies without minds, without feelings, without movement. Even if the structure looks fine, if it doesn’t function, we’re missing the most important piece of the jigsaw called life.
Then graduation comes, and the habit sticks. Too many doctors keep treating living humans as if they’re cadavers waiting for prescriptions. No wonder exercise never makes it into the conversation.
Meanwhile, anyone who actually moves, runners, footballers, gym-goers, has been saying the same thing for eons: it feels good. Movement keeps them sane. It’s therapy without the couch. How psychiatrists manage to miss this universal truth is beyond comprehension.
Medical Colleges: All Brain, No Brawn
Medical colleges drill biochemistry until students can sketch the Krebs cycle in their sleep, but gloss over the fact that moving your body is what keeps the mind afloat. We should be teaching future doctors to sweat, not just memorise pathways. Make them play sports, lift weights, breathe hard. Let them feel what patients need to feel. Only then will they ever take exercise seriously.
I’ve learned more about patient care from my own injuries than from any textbook. Every time I’ve had to rehab myself back from a setback, it’s been a reminder: pain teaches empathy in a way lectures never can.
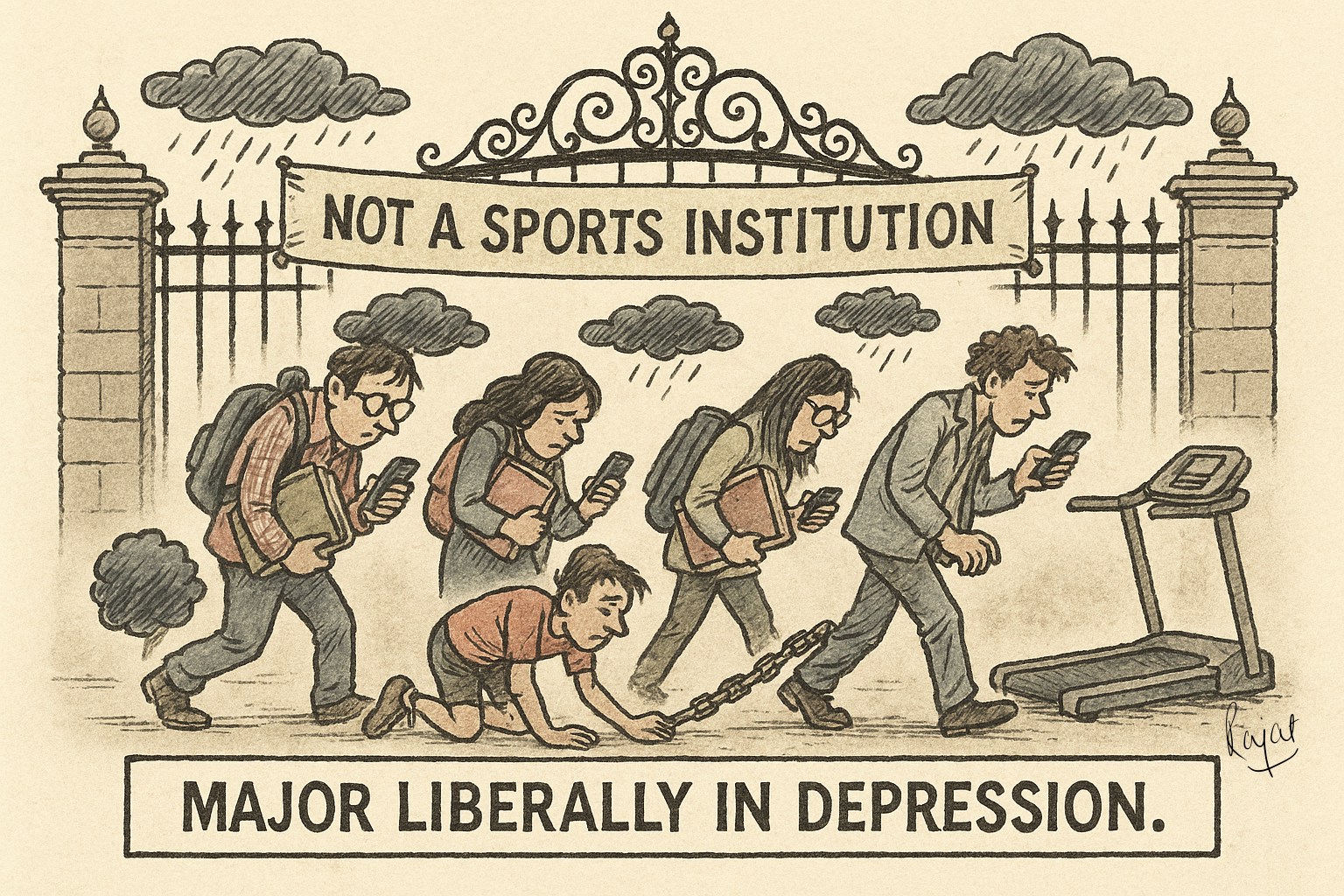
Ivy League Liberal Arts College Majors in Depression
And this allergy to movement isn’t limited to medicine. A decade ago, I asked a premier liberal arts college in India to invest in student sports, not just for medals, but for inclusive participation. The master architect’s reply? “We’re not a sports institution.”
The irony? Their own psychologists admitted that 60% of students showed symptoms of psychological conditions. That was ten years ago. Today, it’s worse. By sidelining sports, they didn’t just cut out games, they practically majored in Entire Depression Studies. Ignore the body, and the mind collapses. Every time.
Prescription: GOYA (Get Off Your Arse)
So here we are. The evidence is overwhelming, yet psychiatrists or psychologists rarely prescribe exercise. If ignoring a proven medication or therapy technique would be malpractice, why isn’t ignoring exercise treated the same?
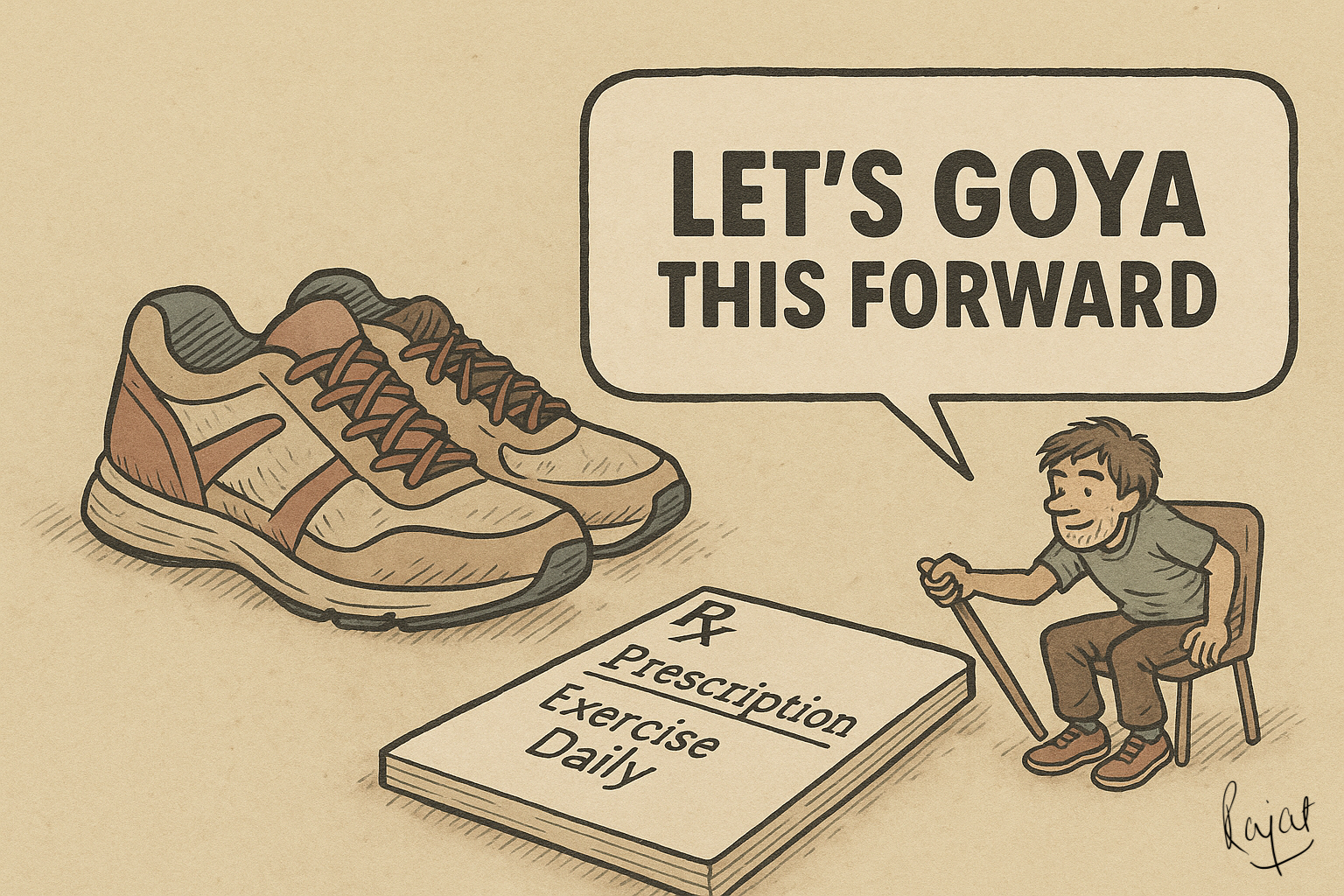
The fix isn’t complicated:
Teach exercise prescription in med schools. I’m ready to help, if you are.
Encourage psychiatrists and psychologists to move themselves. I’ll gladly help structure a program, so you learn not just the theory, but the practice of moving your own backside.
Build referral systems with trainers and physiotherapists. But first, trainers and physiotherapists need to up their game and actually understand exercise, not just for six-packs, but for depression and mental health. I’m happy to design a bridge course, not another jargon-heavy module, but something practical and usable. Basics of exercise science, how to structure safe and progressive programs, how to build habits that actually stick, and most importantly, how to communicate this in plain language to patients. That way, they stop handing out cookie-cutter “3 sets of 10” routines and start delivering movement that heals.
Make exercise reimbursable, like therapy sessions. Insurance companies, are you listening?
And to patients: Don’t wait for the system to catch up. If you’re struggling with depression, pain, or just need to get moving again, reach out. I’ll help you find a place to start, one step at a time.
And above all: stop treating exercise like an optional gummy vitamin. It’s not a hobby. It’s not extra credit. It’s the most powerful prescription we have, and it happens to be fun. Depression isn’t just in the head; it lives in the body too. Healing one without the other isn’t medicine, it’s malpractice dressed up as tradition.
So to psychiatrists, psychologists, professors, policy-makers: stop treating ‘Choley Bhature’ or ‘Gulab-Jamun’ as your warm-up. Lace up, show up, and prescribe movement. I’ll do my bit. You’ve got to do yours.
Because sometimes the best antidepressant doesn’t come in a pill bottle. It comes by GOYA: Getting Off Your Arse.
Let’s Move This Forward
Want to explore one of the ideas I’ve shared here? Whether it’s teaching exercise prescription in medical schools, building bridge courses for trainers and physiotherapists, or finding ways to integrate movement into healthcare, I’d love to hear from you.
And if you’re a patient, this is for you too. Struggling with depression, pain, or simply trying to get moving again? Reach out. Your lived experience is what keeps this real, and I’d be glad to help you take the first step.
Use the form below to get in touch.